Professor of Medicine, Virginia Tech Carilion School of Medicine, Roanoke, Virginia, USA
⚡ Clinical Pearl
Fat tissue increases electrical resistance. Use pure cutting current only (never coagulation) and pre-inject + circumferential incision before snare resection to prevent snare adhesion and perforation.
70-year-old female patient underwent EGD for abdominal pain and intermittent bloating. A large duodenal submucosal lesion was seen (Figure 1). Endoscopic ultrasound showed a submucosal, hyperechoic lesion, consistent with lipoma.
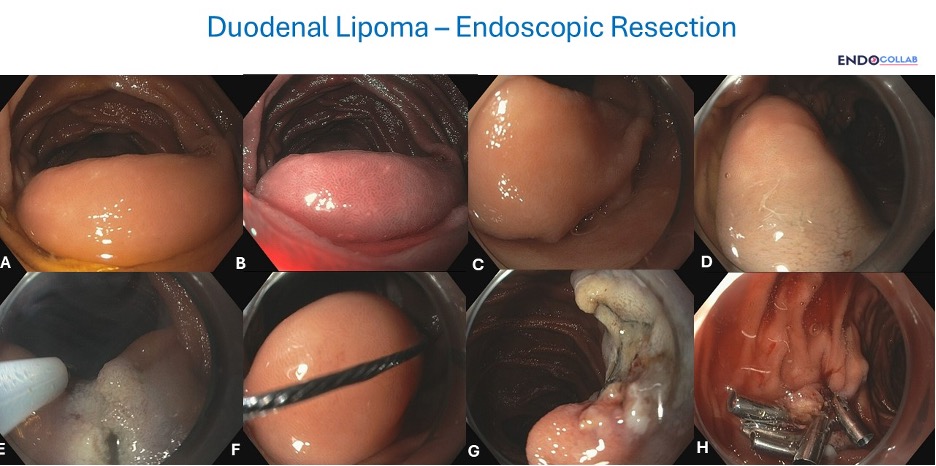
The lesion has characteristic findings of a lipoma: a) yellowish color, b) submucosal location, c) upon applying the tip of closed biopsy forceps the lesion was soft, d) the overlying mucosa was intact (Panel A, B). The latter finding is not always present in lipomas, as these may ulcerate and bleed. As large lipomas like these can result in obstruction, intussusception, gastric outlet obstruction, bleeding and ulceration, a decision was taken to resect it.
Key aspects when resecting a duodenal lipoma:
a) Careful lesion characterization: Evaluate its location in relation to the papilla. Apply air (CO2) and observe its mobility. Use water to determine the location. Examine the base of the lesion. In this case it was semi-pedunculated (Panel C).
b) Avoid straight hot snare resection: Fat tissue decreases electrical conduction, creating resistance to cutting electrical currents and increasing the chances of burning and perforation. There is also risk of the snare getting stuck or glued to the partially cauterized, greasy lesion. For these reasons, we pre-inject the base of the lesion (Panel D) and then perform a hemi- or complete circumferential mucosal and submucosal incision (Panel E).
c) Use pure cutting currents: Once the hemi-circumferential incision and cutting (“pre-cutting”) was accomplished, a snare was used to resect the lipoma using pure cutting currents (yellow pedal) (Panel F). Do not use coagulation current, as this increases the chances of the snare getting stuck to the greasy polyp.
d) Always close the resection site: The duodenum is highly vascularized, and the chances of post-resection bleeding are very high. Additionally, the wall of the duodenum is thin and delayed post-resection perforation may occur, which can be catastrophic. For these reasons, I ALWAYS close the mucosectomy sites in the duodenum using several clips.
References
- Ouwerkerk HM, Raber, Freling G, Klaase JM. Duodenal Lipoma as a Rare Cause of Upper Gastrointestinal Bleeding. Gastroenterology Res. 2010 Dec;3(6):290-292.
- Pei MW, Hu MR, Chen WB, Qin C. Diagnosis and Treatment of Duodenal Lipoma: A Systematic Review and a Case Report. J Clin Diagn Res. 2017 Jul;11(7):PE01-PE05.
- Tjandra D, Knowles B, Simkin P, Kranz S, Metz A. Duodenal Lipoma Causing Intussusception and Gastric Outlet Obstruction. ACG Case Reports Journal. 6(11):e00157, November 2019.
- Phatharacharukul P, Wajid M, Fatima H. Delayed Removal of Entrapped Snare in Colonoscopic Polypectomy. ACG Case Rep J. 2021;8(1):e00535.
Conflict of Interest: None declared.
📚 The Ultimate Guide to GI Bleeding
Dr. Mönkemüller emphasizes mandatory clip closure because duodenal bleeding can be catastrophic. This book gives you the complete hemostasis playbook:
🔬 EndoCollab Premium: The Clinical Case Vault
Cases like this duodenal lipoma appear weekly—with full image series, expert commentary, and technique breakdowns you won’t find in journals.
Una vez resecada, la lesión no parece muy grande. ¿Era necesario el riesgo de la resección?